My secretary's face appeared in the conference room window. I could see from her look that it was the call I was expecting. I excused myself and bolted out of the room. When I stepped outside, she confirmed that my urologist was on the phone. I ran back to my office.
He came to the point immediately: "Andy, you have a tumor. It's mainly on the right side; there's a tiny bit on the left. It's a moderately aggressive one." Then, a bit of good news: "There are only slim odds that it has spread." The whole conversation was matter-of-fact, not a whole lot different than if we had been discussing lab results determining whether I had strep throat.
But what we were talking about was not strep throat. We were talking about prostate cancer.
Let me start at the beginning...
MY FIRST PSA. It all started about a year earlier when my family doctor of 20 years retired. In the fall of 1994, my new doctor gave me a physical exam to establish a new baseline. The physical involved an assortment of blood tests, all of which were in the normal range, with one exception. The test called PSA came back with a result of 5. The acceptable range, according to the lab computer, was 0 to 4.
I didn't know what this test was. In fact, I don't think I'd ever had one before. My doctor's comment was, "It's slightly elevated. It's probably nothing to worry about, but I think you should see a urologist."
He did not seem too concerned, so I didn't get anxious, either. I put off the whole issue without much thought. I did, however, happen to tell one of my daughters, who is a health-care professional. She told a doctor friend of hers, who, it so happens, was just publishing a long article on the pros and cons of screening people with this very same PSA test. Would I want to talk to him about it? I would. I did.
Oh, my God.
With that conversation, I parachuted into the middle of one of the raging controversies of contemporary medicine. Briefly, the issue, as I understood it, seemed to be this: A PSA test (PSA stands for prostate specific antigen) measures a substance emitted both by the normal prostate gland and by cancerous tissue in the prostate gland. Very little escapes from a healthy gland, so elevated PSA readings can be telltale signs of prostate cancer. But just because they can be doesn't mean that they always are.
Telling a person with an elevated PSA that he might have cancer leads him into a system of increasingly complex and uncomfortable diagnostic tests to ascertain whether it is so. If it is, the patient has to make some choices about what, if anything, to do. None of the choices, the friendly voice matter-of-factly explained to me on the phone, are good. None of the treatments work all the time, and all of them have side effects that are unpleasant or worse, like incontinence and impotence.
Anyway, according to my daughter's doctor friend, prostate cancer isn't necessarily fatal. Autopsies show that about half of all men who die of other causes have some cancerous tissue in their prostate. So, my new acquaintance said, why submit unsuspecting men indiscriminately to this test, which only leads to more tests, which then lead to a series of choices, none of which are very good?
He sent me a preprint of his article. It was a scientific medical paper with charts, filled with learned discussion. But I picked up enough of the subtext so that my eagerness to visit a urologist, not very high to start with, waned some more.
It so happened that I was due to leave town on sabbatical in early 1995. I was planning to spend a month in the mountains skiing and writing a book. After a while, the PSA issue worked its way back to my consciousness. Having a computer with me and some time on my hands, I started looking for information on CompuServe. It wasn't hard to find. I found a prostate cancer forum where patients and relatives of patients swapped stories, asked questions of each other, and gave answers. The term PSA was mentioned in every message.
I also found a long review paper in the forum that was written by the head of the urology department at Stanford University, Dr. Thomas A. Stamey. I downloaded it, and I read it from beginning to end.
 I found out some basic facts, such as: Some 200,000 men were diagnosed with prostate cancer in 1994, and 38,000 men were expected to die of it, making it the No. 2 cause of cancer deaths among men (after lung cancer). The paper discussed the seeming paradox of why such a small proportion of the people who have prostate cancer die of it, and speculated that most prostate cancer isn't very aggressive. I wondered, Is it not simply because most prostate cancer is diagnosed in older men who die of other diseases before the prostate cancer has a chance to get them? (This was not encouraging for me. I was only 58 and otherwise in perfect health. I couldn't wave the threat away with such an argument.)
I found out some basic facts, such as: Some 200,000 men were diagnosed with prostate cancer in 1994, and 38,000 men were expected to die of it, making it the No. 2 cause of cancer deaths among men (after lung cancer). The paper discussed the seeming paradox of why such a small proportion of the people who have prostate cancer die of it, and speculated that most prostate cancer isn't very aggressive. I wondered, Is it not simply because most prostate cancer is diagnosed in older men who die of other diseases before the prostate cancer has a chance to get them? (This was not encouraging for me. I was only 58 and otherwise in perfect health. I couldn't wave the threat away with such an argument.)
Then the paper went through the treatment options. My daughter's friend was right. They were all lousy. The most prominent is surgical removal of the tumor. This is done by removing the whole prostate gland, then rebuilding the related internal organs. It's major surgery, with a long recovery and pretty bad side effects. Dr. Stamey's article only hinted at how unpleasant they are. I read a posting on the forum by an airline pilot who had undergone this surgery and was bitter beyond words. He claimed that it cost him his health, his job, and his marriage, and that it ruined his life. It was all very depressing.
But the important thing I took away from this essay was the concept that PSA is a tumor marker. It seemed that the larger the tumor, the higher the PSA. My own result of 5 seemed to correspond to a tumor the size of a sugar cube. I visualized a sugar-cube-sized tumor inside me, and I shuddered.
I came across a mention of a book on prostate cancer, jointly written by a patient and his doctor. I ordered it and when I returned home after my sabbatical, I picked it up. It was quite readable, a thorough and organized review of different treatments, but it was noncommittal. The book itself reflected the contradictions of the literature, without providing guidance as to what course of treatment is best.
I went back and had a repeat PSA test done. As in my case we were looking at a difference in PSA readings of 4 (the upper range of acceptable) and 5, I wondered if the tests were precise enough. So I also decided to test the tests. I had my blood sent to two different labs. Unfortunately, what I hoped for – widely varying results – did not materialize. One test came back at 6.0, the other at 6.1. It appeared that the sugar cube was growing.
These tests ended my procrastination. I made an appointment with a urologist. He first checked my prostate with his finger (this test is called a digital rectal exam, or DRE), and he didn't feel anything. But given my PSA, he did a biopsy a week or so later (not a pleasant experience but not a terrible one either). The biopsy turned out to be positive. Hence the conversation that started with "Andy, you have a tumor."
R&D. I went back to see the urologist. He sat me down and told me my options: surgery, radiation, cryosurgery (in which the tumor is destroyed by freezing it), and, finally, doing nothing and playing the odds. This is euphemistically called "watchful waiting." He told me that in my case "surgery would have a reasonably good chance of getting rid of the tumor." He gave me the impression that the other treatments would have a lower probability of curing me.
He walked me through the complications of surgery, but reassured me: "Don't worry, we can do something about each of those." The examining room walls were covered with posters of contraptions like penile implants and vacuum pumps. I knew that they were devices meant to restore potency, but they evoked images of medieval torture.
I was sent to the hospital to undergo two complex tests. In the first, a bone scan, an instrument scanned my body looking for signs of metastasis – advanced prostate cancer tends to spread to the bones. The second was an MRI, a long and mildly uncomfortable procedure, which looks for evidence of spread into the abdomen. Both were negative, but I got the impression that neither test was all that sensitive, so there might very well be disease that they wouldn't pick up.
I wanted to know more. I called a number of friends who are doctors, who came back with names and phone numbers of prominent practitioners of the different types of treatment. I also decided to dust off my research background and go directly to the original literature. I wrote out the first batch of titles from the bibliography in the prostate cancer book I'd bought, and my wife got copies of these articles from Stanford. My life entered a new routine.
By day, I set up appointments. This was a royal pain. The doctors were hard to get hold of, and when they called back, I was often in meetings, so making one appointment required half a dozen phone calls. By night, I read scientific papers, plotting and cross-plotting the data from one paper with the results from another. As I noted other interesting references from these papers, I would ask my wife to get them on her next trip to the library. This whole exercise reminded me of my younger days, when I did the same thing in the field of semiconductor devices.
Meanwhile, life went on. I had to concentrate on work, which turned out to be a good thing, because it meant I could think about cancer only while I was actually doing my R&D. What suffered was time for sleep. Fortunately, prostate cancer is completely asymptomatic for a long time; my energy level was as good as ever and I was able to keep up with the extra load.
At first, the papers were overwhelmingly confusing. But the more I read, the clearer they got, just as had been the case when I was studying silicon device physics 30 years ago. That added a strange element of enjoyment to a process that was, overall, very scary. I remember how creepy it felt the first time I walked through a hospital door labeled RADIATION ONCOLOGY.
The appointments led to more appointments, the papers led to more papers. A doctor friend ran a computerized search on a number of researchers' names I gave him. From this search I got a bunch of papers that were written in the last six to nine months – written after my reference book was published, in other words. Some of these turned out to be the most significant ones in this whole exercise. The field was hopping, not just with new work and discoveries but with controversy.
Each medical specialty – surgery, cryosurgery, different branches of radiology – favored its own approach. I listened to the audiotape of a long interdisciplinary medical meeting called, appropriately enough, "Prostate Cancer Shootout." I could sense the undercurrents of strong disagreement, couched in polite, faux-respectful terms. I had the impression that the people whose comments I heard had made the exact same comments in meetings before this one and would make them again in the future. The tenors always sang tenor, the baritones, baritone, and the basses, bass. As a patient whose life and well-being depended on a meeting of minds, I realized I would have to do some cross-disciplinary work on my own.
WHAT I LEARNED. The most important thing I learned was that the use of the PSA test reset the entire field of prostate cancer studies. PSA tests went into use only about ten years ago. Their use moved everything forward in time. Typically, a PSA test can indicate the presence of prostate cancer as much as five years earlier than diagnosis by other means, like digital rectal exam.
Not only does this allow for earlier treatment, but it also has an important consequence from a scientific standpoint: We can now learn a lot more about the effectiveness of various treatments by using the PSA test to look for recurrence of the disease. It used to take ten years or more for recurrences to be discovered by DRE and other clinical means. But since PSA can detect recurrence much earlier, the learning process about the effectiveness of treatment is accelerated.
Since the PSA test accelerates the discovery of the tumor in the first place, you have the chance to treat tumors earlier than ever before. One doctor I met told me that all the treatments basically work quite well if you embark on them when your PSA is still relatively low. By contrast, none of them work well if it's high. Being a marker of tumor size, a high PSA suggests that the tumor is large, and a large tumor often extends outside the prostate gland to other parts of the body and can begin the process of metastasizing.
At this point I got a shock. I had an ultrasound imaging test done on my prostate to look for the shape and extent of the tumor. Most ultrasound machines give very ambiguous results, so much so that they are pretty much disregarded as diagnostic tools. But I had this done at a university hospital, where they have a very elaborate, newfangled machine that, in the hands of expert interpreters, supposedly gives more definitive results. In my case, the test suggested that there was a 60% chance that I had extracapsular extension, that is, the tumor extended outside of the prostate gland. I got depressed. Yet I soon found out that this should not have been a surprise at all.
Perhaps the most important paper I came across was a recent study by a group of doctors at Johns Hopkins looking at ten-year results after surgery on some 700 patients. In this study, they correlated the clinical findings – the medical findings on each patient before surgery, such as his PSA, the size of his tumor as established by digital rectal exam, and the biopsy results – with what the pathologists found during surgery. These results were then tabulated. The tables were extremely useful. They allowed me to look up any set of clinical findings and assess the statistical probability of the nature of the cancer in a minute. I had a PSA of 6, with the tumor largely contained in one half of the prostate and found by the biopsy to be moderately aggressive. When I looked up this set of clinical findings in the table, it showed that the chance of my having extracapsular extension was, in fact, about 60%.
The significance of this was contained in a companion paper, which correlated the chance of recurrence of the cancer with the medical observations before surgery. It found that even though the population of patients was carefully selected in terms of being good candidates for surgery, and even though all the operations were performed by one of the best prostate surgeons in the country, many of the patients experienced a recurrence of prostate cancer as indicated by their PSAs starting to rise again. When these patients were classified, the data showed that patients whose cancer was completely contained in the prostate gland experienced the lowest rate of recurrence, patients who had extracapsular extension experienced more frequent recurrence, and patients whose tumor had penetrated other organs near the prostate had an even greater chance of recurrence. I could see in these data what I had been told earlier: Surgery (like everything else) seems to work better at a low PSA.
In my case, if I didn't have any extracapsular extension, the data suggested that if I had a leading surgeon operate on me, I would have only a 15% chance of recurrence in ten years. If I did have extracapsular extension, I would have a 60% chance of recurrence at that time. And I had about a 60% chance of being in the latter class. Computing the odds based on these numbers suggested that my recurrence rate in ten years worked out to about 40%. I wasn't crazy about those odds. Clearly, surgery did not cure everyone, even under the best conditions.
Then there was the question of side effects. As indicated by the CompuServe posting from the airline pilot, these could be pretty bad after surgery. How bad depended on whose data I looked at. According to the surgeons who write papers, the side effects are not so bad. But I also read a study that questioned a large group of patients directly, and those results were alarming: The reports of incontinence and impotence were dramatically worse in the second study, leaving me to wonder whether patients described these things to a third party more pessimistically than to their doctors, or whether patients in the second study were more representative of the work and results of urologists all over the United States, as compared with leading practitioners. In any case, these certainly motivated me to examine other types of treatment.
Prime among these was external radiation. While surgery works by cutting out the tumor along with the rest of the prostate, radiation works by bombarding the area of the prostate, selectively causing more destruction of the cancerous cells than of the healthy ones. There's a lot of controversy about how well this works. Although there seems to be agreement that the side effects associated with radiation treatment are substantially less than with surgery, the effectiveness of the treatment is another issue.
It was especially difficult to get a good handle on the effectiveness of radiation because of the presumption by most urologists that surgery works best. Consequently, younger and healthier patients, particularly patients considered to be good candidates for surgery on account of their tumors being smaller, are selected for surgery, leaving the older, less healthy patients with more advanced tumors to make up the bulk of the patient population that undergoes radiation therapy. The results in the latter class are, of course, worse – reinforcing the spiral that sends the early-stage patients to surgery and the later-stage patients to radiation.
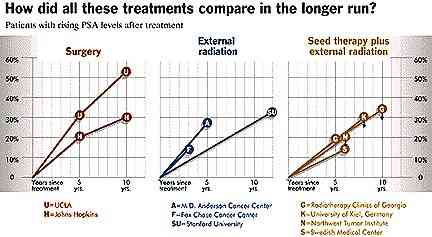
Yet in recent years, as enough patients with lower PSAs have overcome this selection bias and chosen radiation, data have emerged to show that results with radiation are also a lot better when the tumor is treated at an early stage. I came across a study that showed radiation therapy results and related them to the patient's initial PSA. When I took the radiation treatment data and compared them with the surgical data, matching the initial PSAs of the patient populations as best I could, the outcomes were not that different, at least at five years after treatment. (See chart on "recurrence rates.")
When I was doing semiconductor device research, it was expected that I would compare my results with other people's previously published results and that I would comment on any differences. But it seemed to be different in medicine. Medical practitioners primarily tended to publish their own data; they often didn't compare their data with the data of other practitioners, even in their own field, let alone with the results of other types of treatments for the same condition. So I kept on doing cross-comparisons as best I could.
I read about another radiation technique. Radiation can also be delivered to the prostate by implanting radioactive seeds directly into the gland. This was not a new idea. It was tried decades ago and discarded because the results were poor; it seems that the placement of the seeds wasn't uniform enough, leaving "cold spots" between them, and consequently the tumor wasn't completely eradicated.
More recently, however, this technique was being refined. Using ultrasound machines, the doctors could place the seeds far more uniformly and minimize the chances of cold spots. The seeds were left in the body, emitting radiation for six to nine months. The radiation would eventually decay, even though the seeds would stay in place indefinitely. Often the seed therapy (formally called brachytherapy) was combined with external radiation just to ensure that the coverage was complete; even if the seeds should migrate around within the prostate, all parts of the tissue would get some radiation.
While I found references to brachytherapy in my reference book, I could not find any good recent papers on it. I called the technical support department of the manufacturer of the radioactive seeds, and got quite a bit of information from them. The results, at least at five years, looked very good. The technical people also gave me the names of some of the practitioners of this technique. Then, in the middle of my search for information on this subject, a full paper was published that contained ten-year data on hundreds of patients who had been treated by a combination of seeds and external radiation. Unlike most, this paper actually compared the results with the best published surgical results. Basically, the two were very, very similar.
To make matters even more complicated, a doctor friend faxed me an abstract of a presentation describing yet another procedure, a variant of the seed technique called high-dose-rate radiation. In this technique, a highly radioactive seed is attached to a wire that is momentarily inserted into the patient's prostate through a number of hollow tubes, one after the other. The procedure is performed with the patient under local anesthesia. The results in this abstract seemed even better than with regular seed therapy, especially when it came to side effects.
What particularly impressed me about both sets of data was that it seemed few of the recurrences were local, meaning that in the cases in which prostate cancer recurred, it usually didn't appear in the prostate but rather in some distant place in the body. This suggested that these combination radiation therapies are very effective in eradicating the tumor that's in the prostate. If the tumor had already escaped by the time the treatment was given, none of the therapies – not surgery, not any kind of radiation – could be expected to be effective.
The results looked good enough to warrant visits to two practitioners, both in Seattle. One practices seed therapy with the seeds left in; the other one practices high-dose-rate radiation with the seeds inserted for a short time and then removed. There was a logic to the high-dose-rate radiation therapy that really appealed to me. Evidently, one can compute how long the radioactive seed should stay in the prostate. The aim is to achieve a radiation exposure that is matched quite precisely to the size, shape, and location of the tumor. For instance, since the bulk of my tumor was on the right side of the prostate, the therapy could direct more radiation to the probable location of the tumor without having to expose the entire prostate to the higher levels of radiation. It's a programmable technique, customizable to an individual case.
The doctor described high-dose-rate radiation as "smart bombs," while external radiation or even the implanted seeds were more like carpet bombing. This was important because the side effects in the case of radiation come from exposing the neighboring organs, like the urethra and the rectum, to radiation. If one could irradiate the tumor heavily while minimizing the exposure of the other organs, theoretically one should get good results with minimal side effects. In fact, this was consistent with this doctor's results. I sat in his office absorbing the elegance of this technique, and then I turned to him. "If you had what I have, what would you do?" He hesitated. Then he said, "I would probably have surgery." I left, utterly confused – but with some more unpublished data from the two seed doctors that I could add to my charts.
There was one more treatment to consider: cryosurgery. In this technique, instead of cutting the tumor out or blasting it with radiation, doctors freeze the tumor with little coils filled with liquid nitrogen that are inserted in the prostate under anesthesia. I couldn't find any hard data on the results of this technique, and it seemed that the side effects are almost as bad as they are with surgery. I took it out of the running.
I also found that a recent school of thought suggests that both radiation and surgical results can be improved by taking certain testosterone-suppressing hormones that cause the tumor to shrink. The shrunken tumor, I understand, is easier to cut out or to blast away. Since hormones seemed to help both surgery and radiation, I started taking them under the "smart bomb" doctor's suggestion. The hormones had their own side effects, supposedly temporary. I had mild diarrhea and lost all interest in sex.
Meanwhile, I continued with visits to three more well-known surgeons. All were ferociously opposed to the combination radiation therapy, or any radiation therapy whatsoever. One, for instance, suggested the likelihood of a need for a colostomy (this scared me enormously). Another argued that none of these therapies result in zero PSA after treatment, as successful surgery does. This puzzled me. Since some PSA is generated by the prostate tissue itself and radiation does not destroy the prostate tissue, why shouldn't the patient end up with some PSA after treatment? The conversation got so heated that my question was never answered.
Looking for counterarguments, I called up the "smart bomb" radiation oncologist. To my surprise, he took a very evenhanded and unexcited position on the controversy, even as he debunked the specific issues raised. He had never seen a single case of colostomy, for example; he speculated that it may have happened in the very early cases when the rectum was overradiated. With the modern technique, he assured me, in all likelihood that can be avoided.
It sounded good, but I had one last question. "Why," I asked, "would you have surgery done to yourself then?" He thought about it. Finally, he said, "You know, all through medical training, they drummed into us that the gold standard for prostate cancer is surgery. I guess that still shapes my thinking."
I continued with my investigations. I talked to people who had gone through various procedures, including two who had undergone the "smart bomb" procedure. When it was all said and done, I had talked with more than 15 doctors and half a dozen patients. I began to get the same information. I plotted all the relevant data I could find (see "how the treatments compare" chart). It was clear that some cancers recur with the passage of time after all the treatments and that the range of variations for each treatment can be quite broad. It also appeared that whatever recurrences take place come on gradually and that the better the results were at five years, the better they would be at ten.
In any case, it was time for a decision.
DECISION. In July 1995, I went on a week-long bike trip with my wife and some friends. Hours of biking are good to let your mind roam and put a helpful distance between all the mind-numbing data and yourself. I prepared a "balance sheet," first in my mind, then on paper. It looked like this:
Pro: surgery: - It's the gold standard: All these people believe it's the better answer. Can they all be wrong?
- If the tumor is truly contained inside the prostate, it seems to work well.
Pro: seeds plus radiation: - Looks like fewer complications, such as impotence and incontinence. By most accounts it is also easier to go through.
- If my tumor has spread outside the prostate, the radiation can perhaps still get it, as the external radiation covers an area that's larger than the prostate gland.
I looked at the sheet and concluded that if I knew that my tumor was entirely contained, I would go with surgery. On the other hand, if I knew that it wasn't, I would go with the combination radiation. The data said I had about an even chance. I kept riding my bike.
One of the arguments that surgeons tended to make against radiation was that the long-term results – that is, anything longer than ten years – were not as good as in surgery. This wasn't obvious from the data. PSA has only been around for ten years, so as far as I was concerned, both surgery and radiation had relevant data only for ten years or less, and not very much even at ten years. But it occurred to me that if combination radiation, which looked better to me than external radiation by itself, only gave me ten years of freedom from disease, I could buy myself a ten-year reprieve relatively inexpensively, considering that it's a lot less onerous treatment. I have a rule in my business: To see what can happen in the next ten years, look at what has happened in the last ten years. PSA happened in the last ten years, and it is transforming the diagnosis and treatment of prostate cancer. Big things, I reasoned, could happen in the next ten years.
But this argument only worked if the combination radiation treatment gave results comparable to surgery in the first place. All the surgeons said it didn't. The radiologists shyly suggested that it did. I fell back on my data. I looked at my plots. The data said that the treatment results were the same – maybe even better for seeds.
I decided to bet on my own charts. Midway through the week, I confirmed my appointment for high-dose-rate radiation treatment a few weeks later.
TREATMENT. The "smart bomb" doctor said it would help him target his weapons if I had a special MRI procedure done that was more sensitive than the one I had earlier. I lucked out. The university hospital that has this capability was also experimenting with a new technique, in which chemicals injected into the patient's blood interact with the magnetic field of the MRI machine to produce an image of the tumor as a group of red dots superimposed on the image of the prostate. I was awestruck by this technique. I could actually see where the tumor was and, to my relief, I saw no evidence of it being outside the capsule. It was about the size of a sugar cube. I made sure this film arrived at the Seattle doctor's office before me.
Then I headed up to Seattle. I had to check into the hospital at 5:30 in the morning on a Tuesday. Monday was a very hectic day at work, which was wonderful: I didn't have a chance to think about Tuesday at all. But when I settled in on the late-evening flight, the workday behind me, no computers, no phones, the anxiety hit. Although my wife was with me, I didn't feel like talking.
The next morning, I got on the conveyer belt. It was no different than any outpatient procedure: questionnaires and a seemingly unending series of nurses asking very similar questions, taking my temperature, taking blood, on and on. Then, anesthesia. Although it was local anesthesia, it made me zonk out. By the end of the procedure, during which they inserted 16 hollow needles through my crotch into my prostate, I remembered very little of what happened. One incident that stood out involved the attending urologist (the procedure was jointly done by a radiation oncologist and a urologist, who was responsible for placing the hollow needles in the right positions). As I was coming out of my daze, the urologist showed me how he had watched the needle insertion through a fiber-optic cable threaded in my urethra. He described how he could see the needles advancing one after another toward his eyes, as it were. It was very strange.
I was wheeled into a CAT scanner, where they checked the placement of the needles one more time. I later saw the film of my body with the parallel needles in it; it reminded me of a porcupine. They proceeded to do the radiation analysis. Given the shape and size of my prostate, the tumor, and the placement of the needles, they needed to figure out how long the radioactive seed should take traversing in and out of each of the hollow needles. The special MRI came in handy here. The radiation planners were able to use the shape of my tumor as shown by the MRI as the basis for their calculations.
Two youngish guys did the calculations. They didn't look like doctors. They looked as if they could be designing chips at Intel. The calculations went on forever. Tongue in cheek, I asked, "What kind of computer are you using?" I was told, seriously, that they were using a 286, a product that we introduced 13 years earlier and stopped producing four years ago.
Over the next 48 hours, I was wheeled into the radiation room four different times. Each time, a robotic-looking contraption drove the radioactive seed through each of the tubes, one after the other. Then it was all over. They took the needles out. My delighted doctor gave me a high-five and discharged me. The next day I flew home, and the following day I was back at work.
Altogether, I was out of work for three days. After that, for a couple of weeks, things were back to normal. Then the external radiation phase started. This follow-up radiation was done in 28 daily doses, each of which took no more than a few minutes but was a bit of a nuisance.
I showed up at a local hospital every workday morning at 7:30 A.M. I would undress, get radiated, put my clothes back on, and go to work. A week or so into this phase, just as they predicted, I started to get tired in the afternoon. I solved the problem by going home at 4 o'clock, instead of my usual 6:30 or 7 o'clock. I'd take a nap for an hour, wake up, turn on my home computer, and complete my workday at home.
Sometimes I would have a late-afternoon meeting. On those days I checked into a nearby hotel, took my hour's nap, and went back to work as good as new, albeit a bit sheepish about what people might think about my checking into a local hotel in the middle of the afternoon. If they only knew how harmless I was.
To my great annoyance, I gained weight, probably because I had to change my diet. I couldn't eat roughage because of all the bombarding my bowels were getting, so I ate more rich stuff. I gained three or four pounds in five weeks, quite a bit for me.
Then the 28 days were over. I was done. No more hormones, no more radiation, no more naps. In a week or two, I started eating vegetables again, started losing the weight I'd gained, and regained my normal energy. The latter was most important. Three weeks after the end of radiation, I was scheduled to give the keynote speech at Telecom 95 in Geneva, Switzerland. The preparations for the speech were demanding, and the speech itself was the most high-profile of my career. Between Telecom 95 and other activities, I spent two weeks traveling in Europe. All systems functioned just fine. Everything seemed to be back to normal.
Except not quite. Right after radiation ended, I had my PSA checked, the first in a lifelong series of such tests in which they look for recurrence. Even though the results were good, it was a reminder that at least emotionally, things would never be altogether "normal" again.
Half a year and three PSA tests have since passed. My life has been the same as before: my energy, well-being, physical functions (including sex). Still, periodically I have to face the dread of a PSA test. And although the results of the first three tests were very good, I know I will be stuck with this fear for the rest of my life.
SOME CONCLUSIONS. As a result of my progression through the experience of prostate cancer, I arrived at a few conclusions:
• First, tumors grow. Sometimes they grow quickly, sometimes very slowly, but they do grow. I think you should hit a tumor with what you believe is your best shot, early and hard. In my case, it was a combination of hormones, high-dose-rate implant radiation and external radiation. For others, like Senator Dole and General Schwarzkopf, it was surgery. If my best friend had this disease, my advice to him would be, "Investigate, choose, and do – and do it quickly. Be aggressive now. Don't save the best for later."
• All the debates notwithstanding, PSA tests are a godsend. They give you the next best thing to not having cancer: They give you time. I cannot comprehend the arguments reflected by my daughter's doctor friend that we shouldn't do them because the treatment options aren't perfect. Using that same argument, should we not eliminate digital rectal exams? After all, both of them do the same thing: They signal the presence of prostate cancer. PSA just does it earlier.
I feel very strongly that if you are a middle-aged man, you should have this test done regularly; given the rapid rate at which some prostate cancers grow, I would opt for a frequency of once a year. You should know your PSA number just as you know your cholesterol count. Remember, it's a marker. What PSA gives you is the chance to act early. Don't blow it.
I shared what had happened to me and what I'd learned with a handful of friends and close associates. I learned that three of them had elevated PSAs. They were riddled with anxiety but hadn't done anything about it. I ran into another friend who had two relatives with prostate cancer, which greatly increases the likelihood of his getting it himself. Yet he hadn't had a PSA test. When I sit in meetings at work and look at groups of men who are my contemporaries, I want to shout at them, "Do you guys know what your PSA is?"
• There is no good gatekeeper in this business. Your general internist is not; the field of prostate cancer is a complex and changing specialty. Neither is a urologist; urologists have a natural preference toward surgery, perhaps because urologists are surgeons and surgery is what they know best. Any other treatment is deemed experimental even if it has just as much data associated with it. My review of the data led me to conclude that there are viable alternatives.
The whole thing reminds me of the uncomfortable feeling I experienced when I first sought out investment advice. After a while, it dawned on me that financial advisers, well intentioned and competent as they might have been, were all favoring their own financial instruments. I concluded that I had to undertake the generalist's job myself; I had to take the high-level management of my investments into my own hands. Similarly, given the structure of the medical practice associated with prostate cancer, that's the only viable choice any patient has. If you look after your investments, I think you should look after your life as well. Investigate things, come to your own conclusions, don't take any one recommendation as gospel. For starters, know where your case fits in the Johns Hopkins tables – this tells you volumes about your condition. In fact, I think these tables ought to be posted on the walls of every urologist's office. They should be viewed as the point of departure for a prostate cancer patient's bill of rights.
The right answer, in my view, can be arrived at only by comparing the results achieved by the practitioners of all the different treatment forms. This would best be done by cross-disciplinary work. Frankly, I am not impressed by what I encountered of this.
In the paper by Dr. Stamey, the one I downloaded from CompuServe at the outset of my odyssey, he says,"...when faced with a serious illness beyond our comprehension, [each of us] becomes childlike, afraid, and looking for someone to tell us what to do. It is an awesome responsibility for the surgeon to present the options to a patient with prostate cancer in such a way that he does not impose his prejudices which may or may not be based on the best objective information."** I think we have a long way to go to reach this ideal.
**From A.W. Partin and others, Johns Hopkins, Journal of Urology, Vol. 150, pp. 110-14, July 1993.
Copyright 1996 Time Inc. All rights reserved. Used with permission.
|